Our immune system is like a guardian angel, tirelessly working to protect us from unseen threats. When we think of immunity, we often picture vaccines, but that’s just part of the story. Immunology has shaped public health by offering preventive tools like vaccines, early-detection diagnostics, and even solutions for agriculture. By understanding these immunological principles, we can also cultivate plants and grow animal cells in ways that help researchers unlock new scientific breakthroughs. This blog takes you through the wonders of vaccines, diagnostic tech, and cell culture methods—three pillars that bridge health, agriculture, and modern science.
The Basics of Immunology - Defenders and Decoders
How Our Immune System Protects Us
Imagine an army inside your body—always on guard, ready to battle intruders. This immune system has two main branches:
Innate Immunity: Your first responder, providing a quick, blanket defense against any unwelcome pathogen. It acts fast, but it’s not specific.
Adaptive Immunity: This is the expert sniper team. Adaptive immunity, led by T-cells and B-cells, takes longer to mobilize but remembers invaders, so it can fight them faster if they return.
Key Defenders: T-Cells, B-Cells, and Antibodies
Antibodies: These protein soldiers mark harmful invaders so that your immune system can recognize and neutralize them.
T-cells and B-cells: T-cells are the body’s elite cell assassins, while B-cells are more like spies, sending signals (antibodies) to alert the immune system.
Cytokines: These messengers coordinate the immune response, rallying cells to the site of infection.
By understanding these defenders, scientists can develop targeted treatments and tools to boost immunity through vaccines and immune-based therapies.
Vaccines - Training the Body’s Defense Team
The Evolution of Vaccines
Vaccines are the most familiar tool in our immune arsenal, with a long history of saving lives. They train the immune system to recognize and defend against diseases without the risk of infection. The types of vaccines include:
Live-attenuated Vaccines: A weakened form of the pathogen that provides strong, lasting immunity. The MMR vaccine (measles, mumps, and rubella) is a classic example.
Inactivated Vaccines: Made with a killed version of the virus. These vaccines are safer for people with weakened immune systems, such as the polio vaccine.
 |
| Attribution: Volker Vetter, Gülhan Denizer, Leonard R. Friedland, Jyothsna Krishnan, Marla Shapiro, CC BY 4.0 <https://creativecommons.org/licenses/by/4.0>, via Wikimedia Commons |
- Subunit and Conjugate Vaccines: Only specific parts of the pathogen, like proteins, are used. This makes them safer but may require booster shots. HPV and hepatitis B vaccines fall in this category.
mRNA Vaccines - The New Frontier
In recent years, mRNA vaccines have changed the landscape. Instead of injecting a piece of the virus, mRNA vaccines teach cells to make proteins that spark an immune response. The COVID-19 vaccines by Pfizer-BioNTech and Moderna demonstrated how effective this approach can be, especially against rapidly emerging threats. This technology opens the door for vaccines against hard-to-tackle viruses, like HIV and influenza.
Diagnostics - Early Detection for Better Protection
Diagnostics at the Speed of Science
Think of diagnostics as your body’s detectives—identifying health threats even before symptoms show up. Here are some of the key diagnostic tools:
Serological Tests: By detecting antibodies in your blood, these tests can confirm infections like HIV or hepatitis, providing information about past exposure to diseases.
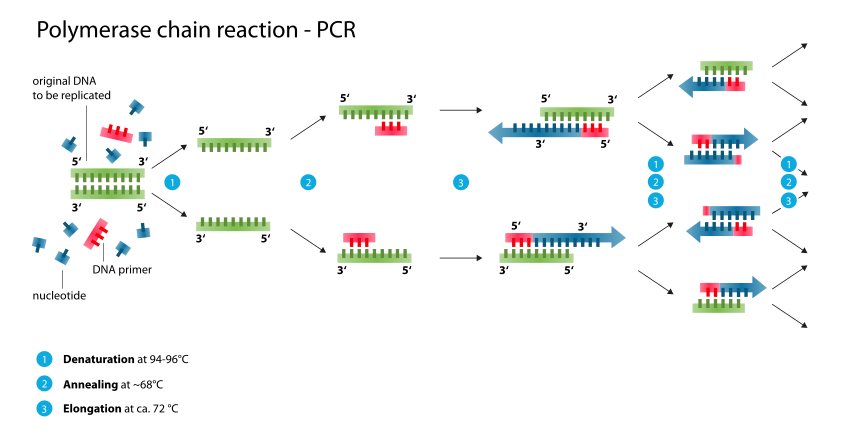
Polymerase Chain Reaction (PCR): PCR works like a copy machine for DNA. It amplifies small amounts of viral or bacterial DNA, allowing for the early detection of infections, as widely seen with COVID-19 tests.
 |
| Attribution: Enzoklop, CC BY-SA 3.0 <https://creativecommons.org/licenses/by-sa/3.0>, via Wikimedia Commons |
- Enzyme-Linked Immunosorbent Assay (ELISA): ELISA detects specific proteins associated with pathogens. It’s useful for diagnosing diseases from malaria to food allergies.
 |
| Attribution: Allan.richard5093, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons |
Cutting-Edge Diagnostic Innovations
CRISPR-based Diagnostics: Originally developed as a gene-editing tool, CRISPR is now used to identify pathogens with precision. Technologies like SHERLOCK and DETECTR detect viral and bacterial genes at a lightning pace.
 |
| Attribution: Domdomegg, CC BY 4.0 <https://creativecommons.org/licenses/by/4.0>, via Wikimedia Commons |
AI and Machine Learning: Algorithms trained on large datasets help detect patterns associated with diseases. In cancer diagnostics, AI is instrumental, especially in image-based detection.
From traditional tools to the latest tech, diagnostic advancements are making it possible to identify and treat diseases with greater speed and accuracy.
Tissue and Cell Culture - Growing Science
Basics of Cell Culture
In a lab, growing cells outside the body might sound like science fiction, but it’s real. Cell culture has helped us understand how cells work, discover new treatments, and even produce disease-resistant crops.
Animal Cell Culture: This method involves isolating cells from an animal and growing them in nutrient-rich media. For example, HeLa cells (human cancer cells) have been used since 1951 in research across nearly every field of medicine.
Plant Tissue Culture: Here, plant cells are grown to regenerate whole plants in lab settings. This method is critical in agriculture to develop plants that can resist disease or pests, conserve rare species, and increase crop yield.
 |
| Attribution: Dorota Paczesniak Dpaczesniak, CC BY-SA 4.0 <https://creativecommons.org/licenses/by-sa/4.0>, via Wikimedia Commons |
How Cell Culture is Shaping Innovation
Genetic Engineering and CRISPR: Scientists use tissue culture for genetic engineering, like CRISPR, to create genetically modified plants or animals with useful traits, such as disease resistance.
3D Cultures and Organoids: Instead of growing cells in a flat layer, 3D culture techniques allow them to form structures resembling organs. Organoids act like miniature organs, helping researchers test drugs and study diseases.
The Future - Immunology Meets Biotechnology
Personalized Medicine and Immunotherapy
Imagine cancer treatments customized just for you. Immunotherapies, such as CAR-T cell therapy, allow scientists to reprogram a patient’s immune cells to target cancer. This personalized approach shows success in treating certain blood cancers like leukemia and lymphoma.
Edible Vaccines and Plant-Based Medicines
By engineering plants to produce vaccine proteins, researchers are developing edible vaccines. Imagine getting vaccinated against diseases simply by eating a genetically modified banana or tomato. This innovation could make vaccines accessible in remote areas without the need for needles or cold storage.
Bioprinting and Organ Regeneration
By combining 3D printing and tissue culture, bioprinting is creating tissue structures for regenerative medicine. This has the potential to provide organs for transplantation, helping address organ donation shortages.
Conclusion: A New Era of Immunity and Biotechnology
Immunology, vaccines, diagnostics, and cell culture methods are redefining health. They’re not only saving lives but also advancing fields like personalized medicine, agriculture, and biotechnology. With AI’s help and biotechnological innovations, we’re on the cusp of even more breakthroughs—bringing us closer to a world where immunity is strengthened, diagnostics are quicker, and the mysteries of biology are unlocked in new ways.
As these fields advance, the synergy between immunology and cell culture will create a future where disease is not only treatable but often preventable. Welcome to the age of scientific possibilities!
